Pattern of Gut Colonization in Infants
Microbial colonization in humans begins at birth and undergoes constant development until 3 years of age till the microbiota becomes adult-like1. Based on the microbial colonization, the gut of an infant also undergoes crucial stages in the development from birth.1 This article reviews the development of the gastrointestinal tract, the composition of gut microbiome and their impact on the health of infants living in low-income countries.
Although gut colonization begins when the fetus descends in the lower uterus, it is completely established only after birth, accompanied by two major transitions. The first transition occurs immediately after birth, during lactation and is dominated by Bifidobacterium. Later, during weaning and introduction of solid foods, Bacteroidetes and Firmicutes dominate the gut2. The early development of gut microbiota depends on several factors such as type of delivery, type of feed (breast vs. formula), use of antibiotics and timing of addition of solid foods2.
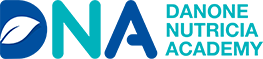
Figure 1: Drivers of gut colonization in infants(Adapted from Milani. et al., 2017)3
Microbial gut colonization in intestine influences the development and physiology of the immune system and impacts health and disease, later in life2. Thus, the first 6 months after birth are identified as a 'window of opportunity', during which contact with certain microbial associated molecular patterns (MAMPs) is crucial for infant gut maturation3.
Development of Gastrointestinal Tract in early life
At birth, the intestinal lumen is aerobic and facilitates the growth of only facultative anaerobes like the Enterobacteriaceae family. Within days, the lumen turns anaerobic and supports the colonization of strict anaerobes such as Bifidobacterium, Clostridium, and Bacteroides1. In the first few weeks, microbial taxa from maternal skin and vagina like Enterococcaceae, Lactobacillaceae, Streptococcaceae, Bifidobacteriaceae, andClostridiaceae dominate the infant's gut.
In the next few months, with infants being on an exclusive feed of milk, oligosaccharide fermenters of milk, like Bifidobacterium propagate and become the most prominent species in this stage1. The intestinal microbiota further changed with weaning and/or the initiation of solid foods made up of complex carbohydrates that cannot be digested by host enzymes. It leads to an increase in Bacteroides, Ruminococcus, Clostridium, and a decrease in Enterobacteriaceae and Bifidobacterium. In the following 12-30 months, the composition of infant gut microbiome shifts towards adult microbiota with a predominance of Ruminococcaceae, Lachnospiraceae, Bacteroidaceae, and Prevotellaceae.
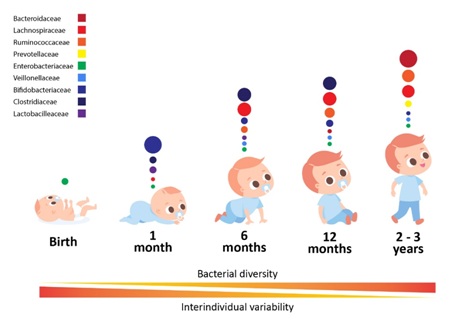
Figure 2: Stages of microbial colonization of the infant and child intestine.
Predominant bacterial families are depicted in circles, where the size of circle is proportional to the relative abundance of bacterial families at each growth stage
(Adapted from Arrieta et al., 2004)1
Composition of the Gut Microbiome
Though a large variation is present at the intraindividual level, the infant’s gut is populated predominantly by the following groups:4
Group 1: Enterobacteriales
Group 2: Bacteroidales and Verrucomicrobiales
Group 3: Selenomonadales, Clostridiales genera Pseudoflavonifracto and Subdoligranum and Deltaproteobacteria Desulfovibrio
Group 4: All Pasteurellales
Group 5: Most of the Clostridiales
Group 6: Clostridiales genera Anaerostipes and Faecalibacterium, Lactobacillales, and Bifidobacteriales
Prevalence of Bifidobacterium in Immunity and Gut
As stated, Bifidobacterium is the predominant species in the infant’s gut4. They belong to the phylum Actinobacteria and were first isolated in 1899 from the fecal matter of a breastfed infant4. Bifidobacterium increases the nutrient absorption in the intestine via producing lactate and acetate and reducing luminal pH3. They also interact directly with the developing immune system and prevent the infant gut by promoting immunological and inflammatory responses, and modulating infant gut mucosal barrier function. The research suggested that improved T-cell response to vaccines and lower neutrophilia at 15 weeks was linked with increased counts of Bifidobacterium species3.
Infant Gut Microbial Colonization in low-income Countries
Children living in low-and middle-income countries (LMIC) are affected by adversities like malnutrition, poverty and maternal stress which can adversely impact the intestinal microbiota. Dysbiosis of the intestinal microbiota is characterized by reduced microbial diversity and increased pathogenic bacteria which may lead to stunting, diarrhea, and malnutrition in children5. Intestinal colonization varies with gestational age. Evidence suggests that LMICs have greater rates of malnourishment with lower rates of breastfeeding. Further, reduced HMOs in the breast milk of mothers may lead to stunting in children5. With a higher incidence of infections in infants and mothers in LMIC, exposure to antibiotics is also likely to be higher. Infants exposed to antibiotics are likely to have lower numbers of Bifidobacterium and Lactobacillus and higher prevalence of phylum Proteobacteria5.
What are the factors to be kept in mind for effective gut colonization in infants in developing countries like India?
- Essential consumption of prebiotics like HMOs
- Reduced use of antibiotics
- Maternal and infant nutrition
Conclusion
Infant gut microbiota is an important factor in governing infant health and affects overall health in the future. Several factors like a vaginal delivery, breastfeeding, and use of antibiotics may impact the composition of intestinal microbiota and thus, infant health6.
References:
- Arrieta MC, Stiemsma LT, Amenyogbe N, Brown EM, Finlay B. The intestinal microbiome in early life: health and disease. Frontiers in immunology. 2014 Sep 5;5:427.
- Tanaka M, Nakayama J. Development of the gut microbiota in infancy and its impact on health in later life. Allergology International. 2017;66(4):515-22.
- Laforest-Lapointe I, Arrieta MC. Patterns of early-life gut microbial colonization during human immune development: an ecological perspective. Frontiers in immunology. 2017 Jul 10;8:788.
- Milani C, Duranti S, Bottacini F, Casey E, Turroni F, Mahony J, Belzer C, Palacio SD, Montes SA, Mancabelli L, Lugli GA. The first microbial colonizers of the human gut: composition, activities, and health implications of the infant gut microbiota. Microbiol. Mol. Biol. Rev.. 2017 Dec 1;81(4):e00036-17.
- Andrews K, Gonzalez A. Contextual risk factors impacting the colonization and development of the intestinal microbiota: Implications for children in low‐and middle‐income countries. Developmental psychobiology. 2019 Jul;61(5):714-28.
- Wall R, Ross RP, Ryan CA, Hussey S, Murphy B, Fitzgerald GF, Stanton C. Role of gut microbiota in early infant development. Clinical medicine. Pediatrics. 2009 Jan;3:CMPed-S2008.