Human milk Immunological component & its effect on immunity through Gut
Human milk acts as a source of complete nutrition for an infant. WHO recommends exclusive breastfeeding for up to 6 months of age and to continue breastfeeding until 2 y of age and beyond with the timely introduction of complementary feeds.
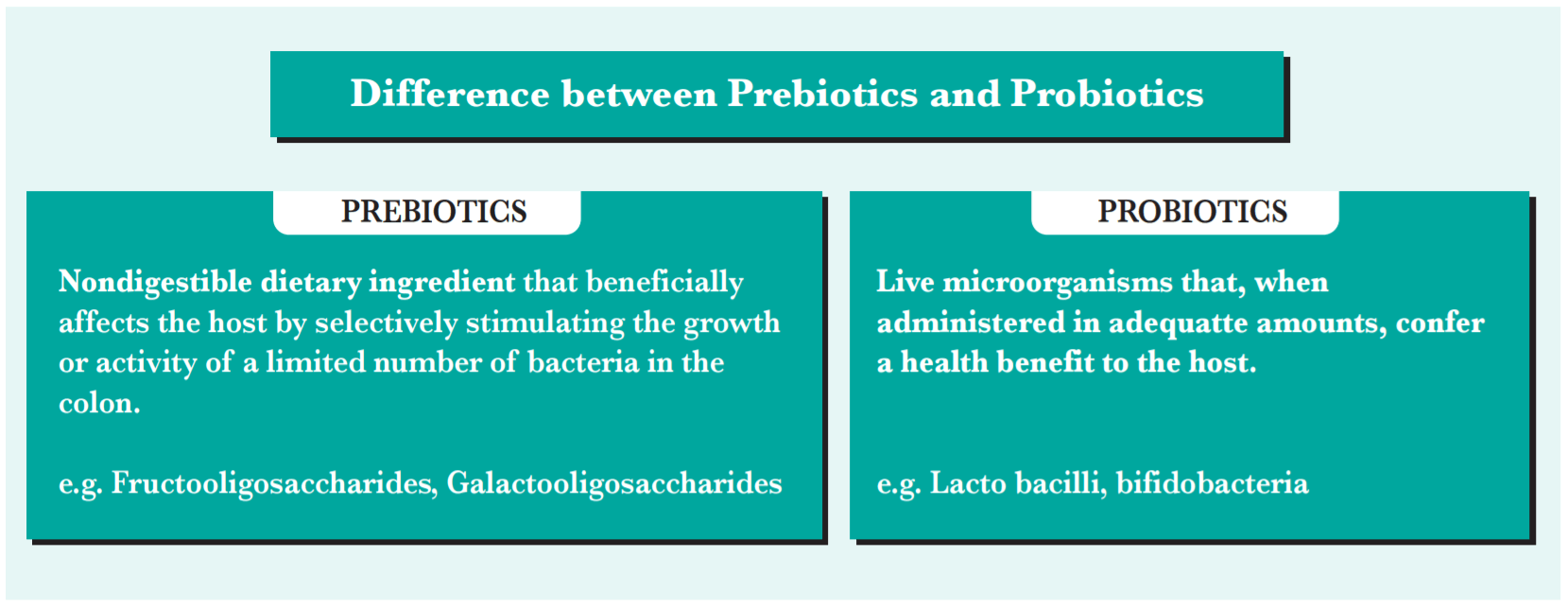
Breast milk contains components that both actively and passively have the ability to modify the immune system of an infant. The highest concentration of immune factors is present in the colostrum and the presence of these are seen throughout the lactation period. It contains all essential macro and micronutrients along with immune factors, hormones, oligosaccharides, probiotics, and other components that influence the infant’s immune system and gut microbiota. Of these, the oligosaccharides (prebiotics) and probiotics present in human milk are the most important factors that help shape the infant's gut. The probiotics largely present in breast milk belong to the genera Staphylococcus, Streptococcus, Lactobacillus, and Bifidobacterium (Mossavi et al, 2018).
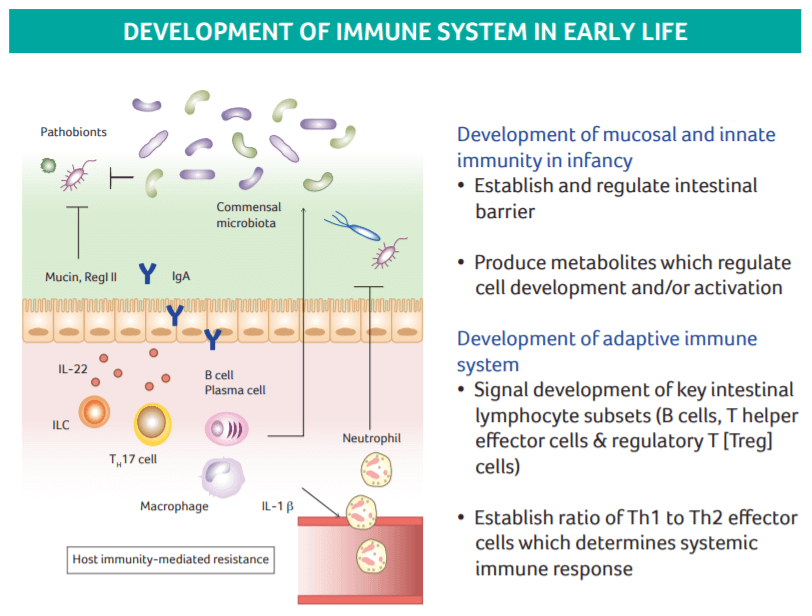
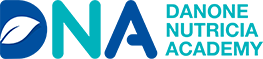
Figure 1 Development of the Immune System in Early Life.
Oligosaccharides, after lactose and lipids, are the third-largest component of breast milk. The concentration of oligosaccharides in breast milk exceeds that of even proteins making it an important nutrient to be studied (Diaz et al, 2018). The highest concentration is found in the colostrum (20-23g/L) and decreases later in the period of lactation to about 12-14g/L in mature milk (Arslanoglu et al, 2008; Bode L, 2012).
They are non-digestible carbohydrate polymer found in breast milk that differs in size, charge, and abundance. It is speculated that there are over 1000 oligosaccharide structures present in breast milk. However, to date, about 200 structures of these oligosaccharides have been identified in pooled human milk samples (German et al, 2010). Oligosaccharides are mainly composed of 5monosaccharides, D- Glucose, D-Galactose, N-Acetylglucosamine, L-Fructose, and N-acetyl neuraminic acid (German et al, 2010; Bode L, 2012).
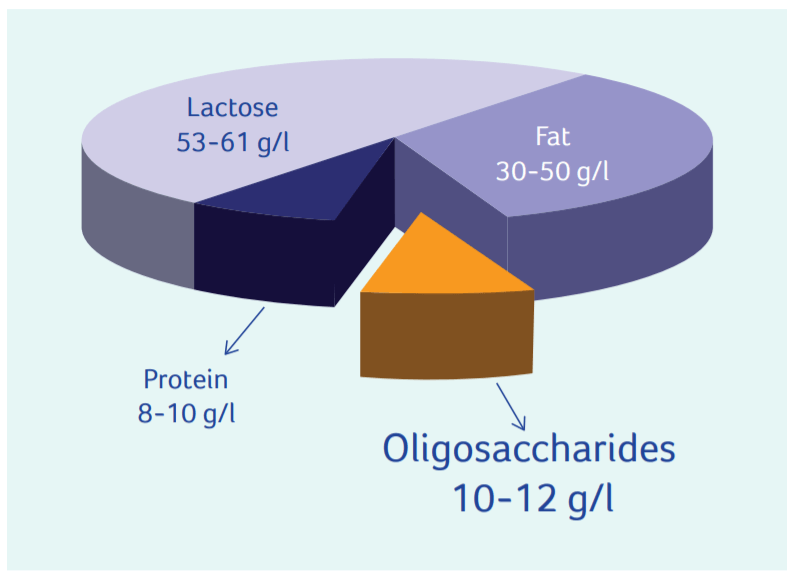
Oligosaccharides cannot be digested by the enzymes present in the small intestine and hence pass undigested to the large intestine wherein it acts as a food for the intestinal microbiota thereby rendering a prebiotic effect. Following are the prebiotic function of oligosaccharides (Doare et al, 2018):
- Promotion of growth of beneficial organisms such as Bifidobacteria (bifidogenesis), especially Bifidobacteria infant is, within the intestinal tract of an infant (Tanaka and Nakayama, 2017; German et al, 2010).
- Establishment of a healthy microbiome by binding with potentially harmful bacteria in the intestinal lumen, asserting direct anti-microbial effect, and modulating the intestinal epithelial immune response.
- Inhibits the adherence of pathogens to the intestinal epithelium by acting as decoy receptors, thereby preventing the pathogen adhesion and invasion of the host cells.
- Helps lower the pH of the intestine, favoring the growth of commensal bacteria and inhibiting the growth of pathogens.
- Alteration of T cell response by balancing the Th1 and Th2 cytokine production.
Infants fed breast milk have a different gut colonization pattern as compared to formula-fed infants (Ho et al, 2018). Lee et al (2015) reported a higher prevalence of Bifidobacteria (70.03%) in breast-fed infants compared to formula-fed infants (40.68%). In particular, B. longum was more abundant in breastfed infants (69.96%) as compared to formula-fed infants (34.17%). Formula-fed infants show a wider spectrum of microbiota, more similar to that seen in adults, as compared to breastfed infants who show a more stable and uniform microbial population (Guaraldi and Salvatori, 2012). The presence of C. difficile, a pathogenic bacterium responsible for 20-40% cases of antibiotic-associated diarrhea, was also low in breastfed infants (Rolfe and Song, 1995). The difference in the intestinal microbiota of breastfed and formula-fed infants can also be seen in the stool patterns. Breastfed infants have larger, softer, and more frequent stools as compared to formula-fed infants.
Even though the microbiota induced by formula feeding is not harmful, it is an attempt to always have formula milk that has a composition as close to breast milk as possible for the benefit of the infant's health, both short and long term. Formula feeds are made by modifying cow’s milk and making it compatible for infant use. However, unlike breast milk, cow’s milk inherently contains negligible amounts of oligosaccharides. The oligosaccharides in milk have a complex structure and therefore identical human milk oligosaccharide structures cannot be synthesized (Arslanoglu et al, 2008). However, understanding the beneficial effect of oligosaccharides on gut health in infants, researchers have tried to develop a non-human milk oligosaccharide as an alternative which still mimics the activities of the oligosaccharides in human milk.
References
- Moossavi et al (2018). The Prebiotic and Probiotic Properties of Human Milk: Implications for Infant Immune Development and Pediatric Asthma. Frontiers in Pediatrics; 6:197 doi: 10.3389/fped.2018.00
- Arslanoglu et al (2008). Early Dietary Intervention with a Mixture of Prebiotic Oligosaccharides Reduces the Incidence of Allergic Manifestations and Infections during the First Two Years of Life. The Journal of Nutrition; 138: 1091–1095
- Tanaka and Nakayama (2017). Development of the gut microbiota in infancy and its impact on health in later life. Allergology International; 66:515e522
- Bier DM, German JB, Lönnerdal B (eds): Personalized Nutrition for the Diverse Needs of Infants and Children. Nestlé Nutr Workshop Ser Pediatr Program, vol 62, pp 13–33
- Bode L (2012). Human milk oligosaccharides: Every baby needs a sugar mama. Glycobiology; 22(9):1147–1162 doi:10.1093/glycob/cws074
- Guaraldi and Salvatori (2012). Effect of breast and formula feeding on gut microbiota shaping in newborns. Frontiers in Cellular and Infection Microbiology; 2: 1-4
- Rolfe and Song (1995). Immunoglobulin and non-immunoglobulin components of human milk inhibit Clostridium difficile toxin A-receptor binding. J. Med. Microbiol; 42:10-19 26. Moro et al (2005). Dietary prebiotic oligosaccharides are detectable in the faeces of formula-fed infants. Acta Pædiatrica; 94(449): 27–30 27. Roberfroid M (2007). Prebiotics: the concept revisited. Journal of Nutrition; 137(3 suppl 2): 830S-7S