Factors Impacting the Developing Gut Microbiota
The large intestine contains at least 30 identified genera and 500 species of microorganisms, making it the largest human reservoir of microbes. The hosts share a complex relationship with the colonizing microbes that affect the development and health of the former.1However, various environmental factors influence the gut microbiota composition, which are discussed in this article.1
Evidence suggests that the composition of infant gut microbiota is idiosyncratic from the first day of life.1 Several factors such as individuality, age, and mode of feeding contribute to the variations in the microbiota.1The number and diversity of the microbial composition in the infant’s gut increase with age.1 The complexity and diversity of the infant gut microbiota composition become similar to that of an adult by around three years of age.1
The gut microbiota plays a critical role in the maintenance of the intestinal barrier function, metabolism, and trophic structure.2 Microbe-host interactions significantly affect host health in later life including infant growth, nutrition, and immunity.2 Dysbiosis in the gut may lead to pathological conditions such as obesity, inflammatory bowel disease (IBD), allergic, and autoimmune diseases.1
Factors affecting GI microbiome development
Several prenatal and postnatal factors influence the initial colonization of the gut microbiota; the major determinants being the mode of delivery, feeding pattern, and antibiotic usage/medication post birth.2
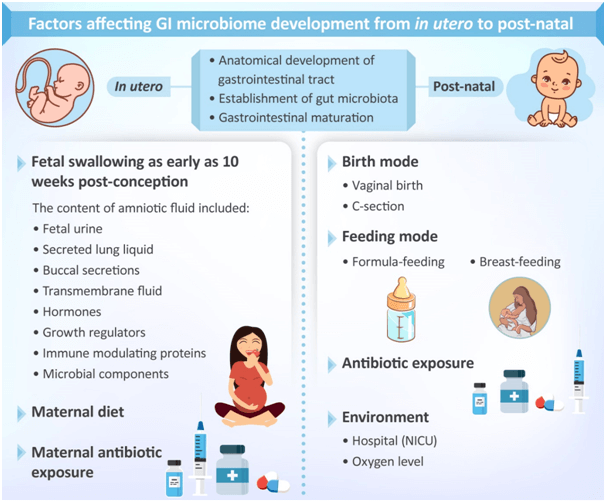
Figure 1: In utero and postnatal factors that influence gut microbiome
(This image has been adapted and recreated from Chong et al., 2018, which is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CCBY) license (http://creativecommons.org/licenses/by/4.0/)1
Mode of delivery
The microbial population to which the infants are exposed is dependent on the mode of delivery. For example, infants born via vaginal delivery are exposed to the microbes present on the mother’s birth canal.1 Lactobacillus and Bifidobacterium, predominantly found in the maternal vaginal canal, usually colonize the gut of the vaginally delivered infants.2,3,4 The influence that environmental factors such as surgical equipment, maternal skin, air, other infants around and healthcare workers have on the neonatal microbiome is greater in case of cesarean delivery.1 Microbes found on maternal skin, Staphylococcus and Streptococcus, initially colonize cesarean delivered infants.2Cesarean delivery may disturb the infant gut microbiota which may affect the microbial-host interactions involved in the development of food tolerance, stress responses, behavior, and metabolism; thus, may lead to long-term consequences such as asthma, childhood obesity, and immune diseases.1,2,5
Gestational age
As compared to term infants, pre-terms are more susceptible to colonization by fewer but more virulent microbes.6 They tend to have high levels of facultative anaerobes such as Enterobacteriaceae, Enterococcaceae, and Streptococcusowing to the high levels of oxygen in the neonatal gastrointestinal tract.1 However, soon the early colonizers reduce the aerobic environment, thus, promoting the growth of obligate anaerobes such as Bifidobacterium, Bacteroides, Clostridium, and Ruminococcus species.1 Gram negative bacteria and multiple-drug resistant (MDR) pathogens are easily acquired and transmitted by neonates and tend to increase the incidence of neonatal intensive care unit (NICU) outbreak.
Preterm infants are often cesarean-delivered which makes them less likely to acquire commensal probiotics such as Bifidobacteria, Lactobacillus, and Bacteroidesfrompassage via the birth canal. Since enteral feeding is also delayed in such cases, acquiring beneficial organisms through breastfeeding is not possible.6
Prebiotics and postbiotics promote the growth of commensal organisms or mimic the commensal activity, thereby exerting beneficial effects.6
Feeding
The newborn is first fed with milk, the composition of which influences the early gastrointestinal microflora.1 The similarity between the microbial composition of the colostrum and the stool samples from the breast-fed infants within the first hour of birth suggests the contribution of feeding type on the early gastrointestinal microflora.1 Different feeding patterns, breast milk or infant feed, can alter the relative abundance of commensal bacteria commonly found in the gut. Compared with breastfed infants, those fed with infant feed tend to have higher levels of facultative, and strict anaerobes.1 However, this difference is lost once weaning starts, the gut microflora of both the breast-fed and infant feed-fed infants evolve to resemble that of an adult.1
Use of antibiotics
Intrapartum antibiotic prophylaxis (IAP) is often administered routinely in mothers delivering by cesarean as compared to in vaginally delivering mothers.8Hence, cesarean delivered term and preterm infants are exposed to antibiotics more often than vaginally born term infants. Few antibiotics that cross the placenta may disturb the neonatal microbiota.1 Antibiotic exposure in mothers and infants during the perinatal period is associated with increased risk of late-onset diseases such as obesity, inflammatory bowel disease, asthma, and other allergic conditions in children.1,9
Moreover, antibiotic pressure may replace the putatively beneficial commensal bacteria with MDR pathogens, which lead to enhanced infectivity.9 Antibiotic therapy may also cause microbial dysbiosis which increases the risk for necrotizing enterocolitis (NEC).10
According to two cohort studies that involved full-term vaginally born infants, the fecal samples from maternal IAP-exposed infants demonstrated reduced alpha diversity than from non-IAP exposed infants.1 In other studies that used 16s rRNA amplicon sequencing, Actinobacteria, Bacteroidetes, and Bifidobacteriaceae in IAP-exposed infants were observed in lower levels while Firmicutes and Proteobacteria were observed in high levels.1
Conclusion
Gut microbiota maturation is a lengthy and complex process that begins in utero and continues after birth.1 The microbial diversity and abundancy in infants depend on various factors such as gestational age, maternal and infant diet, genetics, antibiotic exposure, mode of delivery, etc.1The microbe-host crosstalk is critical for metabolism and immunity, therefore, it is important to understand the impact of the factors that affect the gastrointestinal microbiota and homeostasis.1
References:
- Chong C, Bloomfield F, O’Sullivan J. Factors affecting gastrointestinal microbiome development in neonates. Nutrients. 2018;10(3):274.
- Liu Y, Qin S, Song Y, Feng Y, Lv N, Xue Y, Liu F, Wang S, Zhu B, Ma J, Yang H. The Perturbation of Infant Gut Microbiota Caused by Cesarean Delivery Is Partially Restored by Exclusive Breastfeeding. Frontiers in Microbiology. 2019 Mar 26;10:598.
- Freitas AC, Hill JE. Bifidobacteria isolated from vaginal and gut microbiomes are indistinguishable by comparative genomics. PloS one. 2018 Apr 23;13(4):e0196290.
- Huurre A, Kalliomäki M, Rautava S, Rinne M, Salminen S, Isolauri E. Mode of delivery–effects on gut microbiota and humoral immunity. Neonatology. 2008;93(4):236-40.
- Eggesbø M, Mandal S, Midtvedt T. Factors affecting infant gut microbiota and possible consequences for health. Microbial ecology in health and disease. 2015;26.
- Patel RM, Denning PW. Therapeutic use of prebiotics, probiotics, and postbiotics to prevent necrotizing enterocolitis: what is the current evidence?. Clinics in perinatology. 2013 Mar 1;40(1):11-25.
- Folgori L, Tersigni C, Hsia Y, Kortsalioudaki C, Heath P, Sharland M, Bielicki J. The relationship between Gram-negative colonization and bloodstream infections in neonates: a systematic review and meta-analysis. Clinical Microbiology and Infection. 2018 Mar 1;24(3):251-7.
- Stinson LF, Payne MS, Keelan JA. A critical review of the bacterial baptism hypothesis and the impact of Caesarean delivery on the infant microbiome. Frontiers in Medicine. 2018;5:135.
- Bhalodi AA, van Engelen TS, Virk HS, Wiersinga WJ. Impact of antimicrobial therapy on the gut microbiome. Journal of Antimicrobial Chemotherapy. 2019 Jan 1;74(Supplement_1):i6-15.
- Staude B, Oehmke F, Lauer T, Behnke J, Göpel W, Schloter M, Schulz H, Krauss-Etschmann S, Ehrhardt H. The microbiome and preterm birth: a change in paradigm with profound implications for pathophysiologic concepts and novel therapeutic strategies. BioMed research international. 2018;2018.