Analysis of bifidogenic effect in infants fed formula with scGOS:lcFOS
Background
It is now known that gut is the largest immune organ housing about 70%-80% immune cells of the body. The gut microbiota is one of the most important factors in regulation of immune response. Newborn infants are believed to have a sterile gut. Post birth, several environmental factors such as diet, especially in the early months of life, have a pivotal role to play in shaping of the gut microbiota. The developing indigenous microflora helps protect the infant against the invading pathogenic microorganisms.
The gut of a breastfed infant is predominantly present in Bifidobacteria and Lactobacilli species. This could be attributed to the presence of a high level of complex oligosaccharides (10-12 g/L) present in breast milk, which exert a prebiotic effect and promote the growth of commensal organisms such as Bifidobacterium in infants. The healthy gut microflora ferments the available prebiotic oligosaccharides to produce short-chain Fatty acids (SCFAs) such as acetate, propionate, butyrate and lactate in the colon.
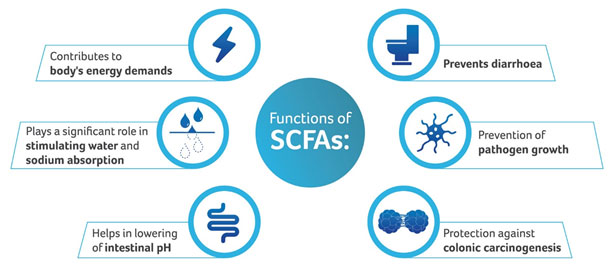
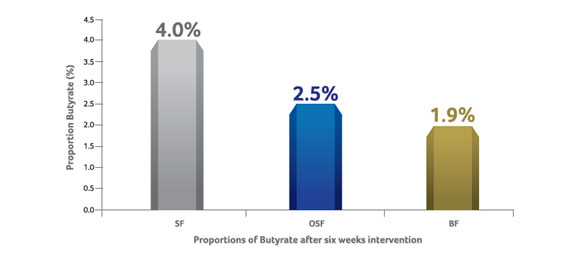
SCFA pattern and its changes are reflective of the bacterial composition of the gut. The faeces of breastfed infants contains mainly acetic and lactic acid with little or no propionic and butyric acid. On the contrary, Faeces of Formula-Fed infants predominantly contain acetic and propionic acid with little amounts of butyric acid.
Recently, the bifidogenic effect of a prebiotic mixture 90% galacto-oligosaccharides (GOS) and 10% fructo-oligosaccharides (FOS) mimicking the molecular size, distribution and function of prebiotic oligosaccharides found in human milk has been demonstrated.
Aim:
The study was conducted to investigate whether an infant Formula supplemented with scGOS:lcFOS was associated with a bifido-dominant flora, not only in bacterial numbers but also with respect to the

metabolic activity of the colonic microbiota, as measured by:
Study Design:
A randomized, double blind placebo-controlled intervention trial with 2 intervention groups was characterized by the following:
|
Particulars |
Characteristics |
|
Participants |
60 formula fed infants |
|
Age |
7 – 8 weeks post birth |
|
Birth weight |
2600 – 4500 g |
|
OSF group |
Supplemented with 0.8 g/100 ml
galacto-oligosaccharides (GOS) and fructo-oligosaccharides (FOS) in a ratio
of 9:1 [n=24] |
|
SF group |
Standard Formula without prebiotics [n=23] |
|
BF group |
Breastfed infants included as reference group
[n=21] |
OSF: oligosaccharide formula; SF: standard formula; BF: breastfed
Faecal samples were collected as Freshly as possible within 3 days of initiation of the intervention, at 4 weeks and at the end of the study period (6 weeks) for the number of Bifidobacteria, pH, short-chain Fatty acids and lactate.
Result and discussion:
The study demonstrated that a mixture of scGOS:lcFOS infant milk formula in a 9:1 ratio was able to selectively stimulate the growth of Bifidobacteria with associated changes in faecal pH and SCFA content in fully formula-fed infants aged 4 to 12 weeks.
The study was the first to demonstrate the bifidogenic effect and an associated change in metabolic activity with the use of scGOS:lcFOS supplemented Formula in infants with a pre-established microflora associated with conventional milk formula.
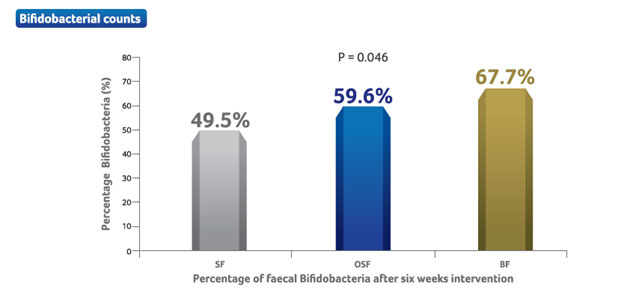
- After 6 weeks, the mean proportion of Bifidobacteria was significantly higher in the OSF group (59.6% versus 49.5% in the SF group).
- The difference between the 2 study groups was statistically significant (P = 0.046).
Note: Baseline percentages were 45.2% and 47.3% for the OSF group and SF group respectively, without correction for the model.
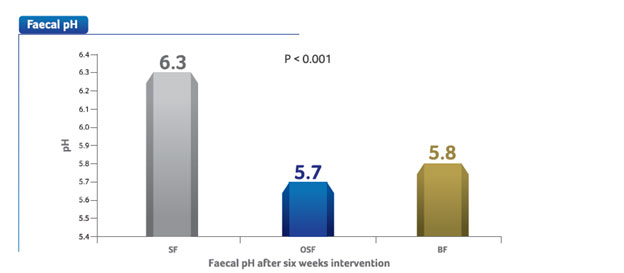
- The mean pH in the OSF and SF groups were 5.7 and 6.3 respectively.
- The difference between the OSF group and the SF group is statistically significant (P <0.001). The pH of faeces of the breastfed reference group was 5.8.

- Production of short-chain-fatty acids and a decrease of the luminal pH has been attributed to bacterial fermentation of non-digestible carbohydrates and proteins in the colon.
- Lowering of luminal pH is favorable for the growth of commensal organisms and discourages the growth of pathogenic organisms.
Note: Baseline values for faecal pH were 6.1 and 6.3 for the OSF group and SF group respectively.
- Acetic acid was the main SCFA produced accounting for about 85% (OSF) and 77% (SF) of the total SCFA's and the difference between the 2 groups was statistically significant (P < 0.001).
- Propionic acid was significantly lower in OSF group as compared to SF group (P < 0.001).
- The SCFA pattern of infants in the OSF group, approximates the pattern of the SCFA's of infants in the BF group. Significant increase in lactate levels in the OSF group (P < 0.001) was observed.
- The difference in SCFA pattern between OSF and SF groups indicates a difference in gut microbiota composition, which is
- consistent with the higher bifidobacterial counts observed in the OSF group.
- Production of acetic and lactic acid is attributed to presence of Bifidobacteria and Lactobacilli in the colon of breastfed infants.
- Propionate and butyrate are commonly found in adults and Fermentation profile in SF group indicates more adult like colonic microflora.
- Bifidobacteria is responsible for the production of L-Lactate. The increase in Bifidobacterium counts reflect the shift towards higher L-Lactate levels observed in the OSF group
Conclusion:
- A healthy microflora is very important for the general well-being of an infant since it plays an important role in normal nutrition and metabolism.
- The trial showed that Feeding a Formula containing prebiotic scGOS:lcFOS oligosaccharides to Formula-Fed infants with an established intestinal microflora results in an increased proportion of Bifidobacteria in the stools.
- This modification of the microflora was associated with a reduction in stool pH and a SCFA pattern containing a higher proportion of acetate and a lower proportion of propionate.
- The changes induced by scGOS:lcFOS brings the intestinal flora and its metabolic activity closer to that of breastfed infants.
Key findings:
Supplementation of an infant formula with a prebiotic mixture of oligosaccharides (scGOS:lcFOS) in the ratio of 9:1 helps:
- Stimulate growth of Bifidobacteria
- Lower the luminal pH
- Significantly increase the levels of lactate
- Modify the intestinal flora and bring the metabolic activity closer to that of breastfed infants
References:
- Knol J., Scholtens P., et al. Colon microflora in infants fed formula with galacto- and fructo-oligosaccharides more like breast-fed infants. J Pediatr Gastroenterol Nutr. 2005Jan;40(1):36-42.
IMPORTANT NOTICE:
Breast milk is best for babies. At Danone, we support breast feeding and believe that breast milk is the best food for babies as the sole source of nutrition for the first 6 months of life and is recommended to be continued until 2 years with the introduction of appropriate complementary foods after 6 months of age.
MOTHER’S MILK IS BEST FOR YOUR BABY
The World Health Organization (WHO)* has recommended that pregnant women and new mothers be informed of the benefits and superiority of breast-feeding, in particular, the fact that it provides the best nutrition and protection from illness for babies. Mothers should be given guidance on the preparation for and maintenance of lactation, with special emphasis on the importance of the well-balanced diet both during pregnancy and after delivery. Unnecessary introduction of partial bottle feeding, or other foods and drinks should be discouraged since it will have a negative effect on breast-feeding. Similarly, mothers should be warned of the difficulty of reversing a decision not to breastfeed. Before advising a mother to use an infant formula, she should be advised of the social and ¬financial implications of her decision. For example, if a baby is exclusively bottle-fed, more than one can (500g) per week will be needed, so the family circumstances and cost should be kept in mind. Mother should be reminded that breast milk is not only the best but also the most economical food for babies. If a decision to use infant formula is taken, it is important to give instruction on correct preparation methods, emphasizing that unboiled water, unsterilized bottles or incorrect dilution can lead to illness.
*See: International Code of Marketing of Breast Milk Substitutes, adopted by the World Health Assembly in Resolution WHA 34.22, May 1981.
Importance of Breastfeeding:
(i)Immediately after delivery, breast milk is yellowish and sticky. This milk is called colostrum, which is secreted during the first week of delivery. Colostrum is more nutritious than mature milk because it contains more protein, more anti-infective properties which are of great importance for the infant's defense against dangerous neonatal infections. It also contains higher levels of, Vitamin 'A', (ii) breast miIk- A) is, a complete and balanced food and provides all the nutrients needed by the infant [for the ¬first six months of life] (B) has anti-infective properties that protect the infants from infection in the early months (C) is always available; (D) needs no utensils or water (which might, carry germs) or fuel for its preparation, (iii) breastfeeding is much cheaper than feeding infant milk substitutes as the cost of the extra food needed by the mother is negligible compared to the cost of feeding infant milk substitutes, (iv) mothers who breast-feed usually have longer periods of infertility after child birth than non-lactators; (b) details of management of breast feeding, as under:- (i) breast-feeding- (A) immediately after delivery enables the contraction of the womb and helps the mother to regain her -figure quickly; (B) is successful when the infant suckles frequently and the mother wanting to breast-feed is confident in her ability to do so (ii) in order to promote and support breast-feeding the mother’s natural desire to breast feed should always be encouraged by giving, where needed, practical advice and making sure that she has the support of her relatives. (iii) adequate care for the breast and nipples should be taken during pregnancy. (iv) it is also necessary to put the infant to the breast as soon as possible after delivery, (v) let the mother and the infant stay together after the delivery, the mother and her infant should be allowed to stay together (in hospital, this is called "rooming-in"); (vi) give the infant colostrum as it is rich in many nutrients and anti-infective factors protecting the infants from infections during the few days of its birth; (vii) the practice of discarding colostrum and giving sugar water, honey water, butter or other concoctions instead of colostrum should be very strongly discouraged; (viii) let the infants suckle on demand; (ix) every effort should be made to breast-feed the infants whenever they cry; (x) mother should keep her body and clothes and that of the infant always neat and clean.
Breast-feeding is the best form of nutrition for babies and provides many benefits to babies and mothers. It is important that, in preparation for and during breast-feeding, you eat a healthy, balanced diet. Combined breast and bottle-feeding in the ¬first weeks of life may reduce the supply of your own breast-milk and reversing the decision not to breast-feed is difficult.
Always consult your Healthcare Professional for advice about feeding your baby. The social and financial implications of using infant formula should be considered. Improper use of an infant formula or inappropriate foods or feeding methods may present a health hazard. If you use infant formula, you should follow manufacturer's instructions for use carefully - failure to follow the instructions may make your baby ill.
Published by:
Nutricia International Private Limited
Building A, unit no. 304, 3rd Floor,
Agastya Corporate Park, Kamani Junction,
L.B.S. Marg, Opp. Fire Brigade,
Kurla (West), Mumbai 400070
CVM code: 1579155076138