Important Notice
If you are a doctor, dietitian, nurse, pharmacist, then click on I’m a healthcare professional to proceed. For persons other than Health care professionals, we request you to visit www.danone.in.
Intestinal colonisation is a stepwise process during the neonatal period as it depends on mode of delivery, environmental factors, bacterial interactions and the host itself, resulting in colonisation with a complex heterogenous bacterial flora. In comparison with term infants, preterm infants are vulnerable to infections and have a weaker immune system because there is a delay in the establishment of a bifidogenic flora.
The influence of prematurity of their intestine is not as important as the influence of extrinsic factors such as type of feeding, antibiotic treatment and the nosocomial environment of these infants during intensive care. One such extrinsic factor is – feeding, which is important during the initial stages of life and for quality of intestinal colonisation of feeding.
Breast milk is the ideal nutrition during early infancy that seems to favour a more diverse microflora with dominance of Bifidobacteria and Lactobacilli. Human milk oligosaccharides (HMOs) have been identified and researched upon, they are found to be resistant to enzymatic digestion in the upper gastrointestinal tract, which is a prerequisite for producing a prebiotic effect. Various studies have reproduced the prebiotic effect of HMOs by using a specifically composed prebiotic mixture of scGOS:lcFOS in the ratio of 9:1 in such a way that the size distribution of the molecules is similar to that of HMOs, therefore containing 90% of the low molecular mass galacto-oligosaccharides and 10% of the high molecular mass fructo-oligosaccharides. This composition consists of galacto-oligosaccharides derived from lactose and fructo-oligosaccharides extracted from chicory roots with a reduced amount of the low molecular mass fraction. It has been observed that this combination promotes beneficial intestinal bacteria in a synergistic way so that a maximum number of different species, especially Bifidobacteria and Lactobacilli can grow in the infant gut.
This study explores the effect on the faecal microflora of supplementing a preterm formula with such an oligosaccharide mixture, with respect to Bifidobacteria, in preterm infants.
To investigate the effects of preterm formula containing scGOS:lcFOS (9:1) on the faecal microflora and stool characteristics of preterm infants.
A randomised-controlled intervention study of 30 healthy preterm infants, with maximum gestational age of weeks, were randomly assigned to 1 of 2 formula groups:
| Study group | |
|---|---|
| Control group | Standard infant formula without scGOS:lcFOS (n=15) |
| Test group | Infant formula with scGOS:lcFOS 1g/100ml (n=15) |
| Reference group | Infants on breast milk + HMF (n=12) |
The first day of full formula feeding was defined as measurement day 1. Measurements were repeated after 7, 14 and 28 days. On each of these days, microbiological analysis of faecal flora, stool characteristics and possible side effects were recorded.
For all infants, enteral nutrition was started with pasteurised mother’s milk. When a volume of 80 ml/kg/day was tolerated, the milk was supplemented with a commercially available human milk fortifier (HMF). When the neonatologist incharge decided to start formula feeding because the mother was no longer able to provide milk, the infants were randomly assigned to one of two formula groups.
The prebiotic oligosaccharide mixture of scGOS:lcFOS in the ratio of 9:1, significantly stimulated the growth of Bifidobacteria. The increase in the number of faecal Bifidobacteria was accompanied by increased stool frequency and softer stools.
Bifidobacterial count
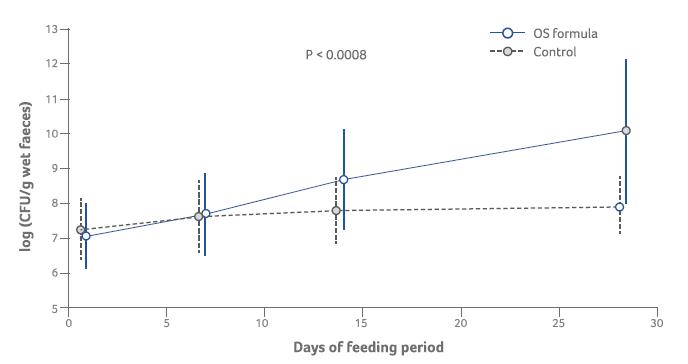
Number of bifidobacteria
Stool characteristics
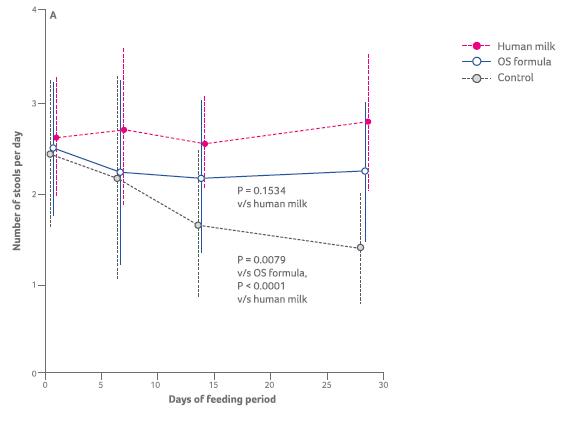
Stool frequency
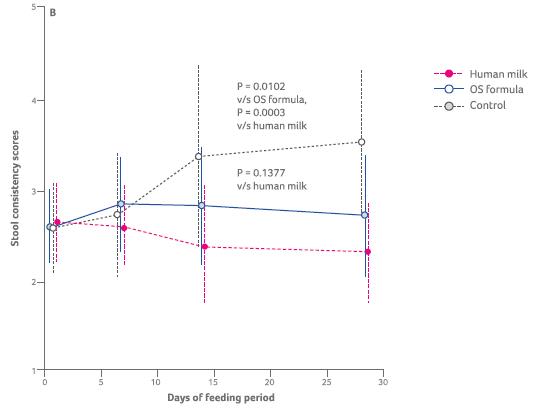
Stool consistency