Preterm Infants: Incidence, prevalence, and burden
Preterm birth (PTB) is defined by the World Health Organization (WHO) as the birth of a baby before 37 weeks of gestation. Preterm birth is among the top two causes of child mortality worldwide, accounting for more than a million deaths per year. 6-7% of the babies born in industrially advanced countries are preterm.1 Preterm babies often are born with very low (less than 1.5 kg) or low birth weight (less than 2.5 kg). Very low or low birth weight babies pose major risk of hypothermia and need intensive care facilities, to reduce mortality risks. They are also more susceptible to non-communicable diseases, later in their life.2
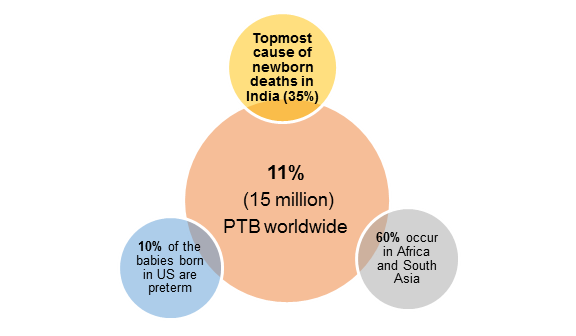
Prevalence of PTB
PTB is a major clinical and public health issue that affects people all over the world.1,2 .
Global burden of PTB:
The global burden of PTB is enormous, with frequent need for intensive care hospitalizations, leading to an emotional and financial burden. Following data elucidates the global burden of PTB.1,2
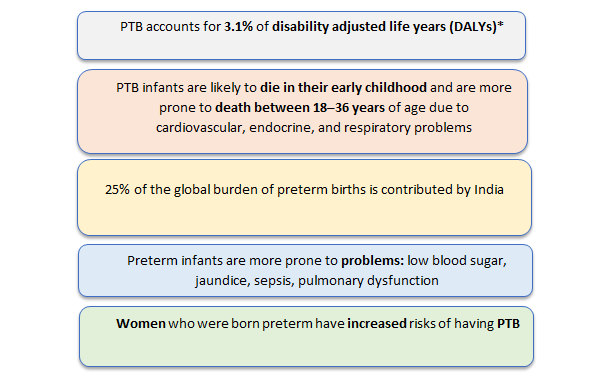
*Disability Adjusted Life Year (DALY): One DALY represents the loss of the equivalent of one year of full health. DALYs for a disease or health condition the sum of the years of life lost (YLLs) due to premature mortality and the years lived with a disability (YLDs) due to prevalent cases of the disease or health condition in a population (WHO).
Risk factors associated with preterm birth
Many factors increase the risk of preterm birth. They are broadly categorized into six groups, as shown below.2
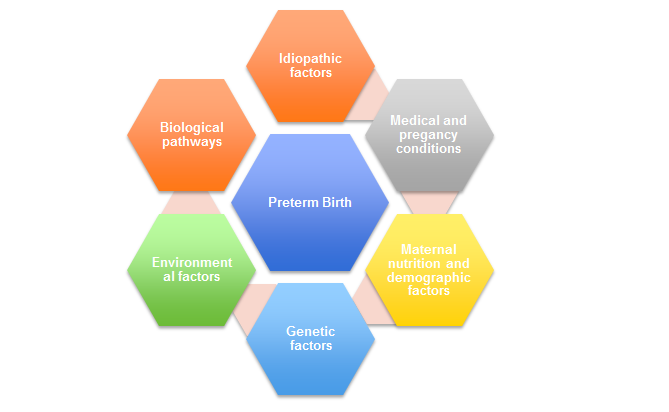
Maternal nutrition and sociodemographic factors2
Most maternal demographic factors include age, race, socio-economic status, educational and marital status. Also, lower socio-economic strata, younger in age and academic level, are more susceptible to delivering preterm babies. Nutritional deficiencies like vitamin D, folate, or iron are significant contributors to PTB. Women suffering from sexual abuse, anxiety, depression are at more risk of delivering preterm babies.1
Medical conditions1
Pregnancy conditions such as multiple gestations, short intervals between pregnancies, previous PTB history predispose women to PTB. Also, medical conditions such as hypertension, thyroid disorders, diabetes increase the risk in women.
Genetic factors
Genetic factors play a significant role in PTB predisposition. Women who were born preterm, women with sisters having PTB experience have a higher prevalence of PTB.1
Environmental factors
Factors such as pollutants and xenobiotics exposure, increased use of agricultural pesticides and herbicides increase the incidence of PTB.1
Biological mechanisms
Several biochemical factors playing a crucial role in PTB pathogenesis are inflammatory responses, maternal-fetal hypothalamo-pituitary adrenal activation, uterine overdistension, etc. Microbial infections, especially intrauterine or of the lower genital tract, are a significant risk factor for PTB.1
Idiopathic factors
Some causal factors are defined poorly for PTB due to its multifactorial nature. Only 50% of the causes of PTB are well defined, while the rest are idiopathic.1
Post-birth complications in preterm babies
Extremely premature infants’ survival rate has risen in the last two decades. Prematurity complications also have become common as more infants survive. Immaturity of multiple organs places preterm babies at higher risk for various complications during their time in newborn intensive care units (NICUs). A list of potential preterm birth complications is given below.3
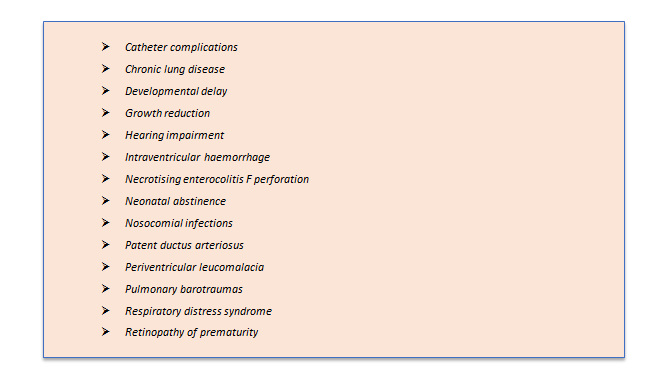
Central nervous system (CNS) complications
Brain lesions are among the adverse neonatal outcomes. Incidence of intraventricular hemorrhage (IVH) is found to be inversely proportional to gestational age. Taking ahead, about 15% of infants with grades I–III IVH develop grade IV IVH or periventricular hemorrhagic infarction (PVHI). Additionally, periventricular leucomalacia (PVL)is found more in extremely premature infants.3
Necrotising enterocolitis (NEC)
Necrotizing enterocolitis is an inflammatory disorder ofthe gastrointestinal tract. It is 100 times more frequentin premature neonates than in term neonates.In 22–50% of cases, NEC progresses to short bowelsyndrome (SBS), making it the leading causeof SBS in infancy.3
Pulmonary complications
Preterm babies often face severe neonatal lung disease. The causes can be due to structural immaturity, surfactant deficiency, and infection.3 Preterm birth also manifests as respiratory distress syndrome (RDS). Infants with RDS often need invasive and non-invasive respiratory support, oxygen supply and surfactant replacement therapy. Subsequently, few RDS infants pose a risk of developing chronic lung disease of prematurity, abnormal respiratory function and increased respiratory morbidity through childhood and into adult life4
Apart from these, premature infants also have a risk of major and minor disabilities such as impaired cognition and speech, cerebral palsy, psycho-social and behavioral disorders, motor and visual defects, and dysfunction at school.5
Conclusion
PTB is multifactorial, with 50% of that being the idiopathic symptoms. Deficits in understanding the etiology limits the prediction of spontaneous PTB. Several factors such as infections, socio-economic and maternal factors, and genetic factors are important determinants of PTB. Preterm births are at a long-term risk of developing complications such as- chronic lung disease, growth reduction, impaired vision and hearing, cerebral palsy, and other developmental defects. Addressing the etiology of PTB will help establish early interventions to avoid its incidence.
References
- Sheikh IA, Ahmad E, Jamal MS, Rehan M, Assidi M, Tayubi IA, AlBasri SF, Bajouh OS, Turki RF, Abuzenadah AM, Damanhouri GA. Spontaneous preterm birth and single nucleotide gene polymorphisms: a recent update. BMC genomics. 2016 Oct;17(9):39-50.
- Ministry of health and family welfare. Government of India. India newborn action plan. [Online]. Available at: https://www.newbornwhocc.org/INAP_Final.pdf. Accessed on:11/5/2017.
- Ward RM, Beachy JC. Neonatal complications following preterm birth. BJOG: An International Journal of Obstetrics & Gynaecology. 2003 Apr;110:8-16.
- Course C, Chakraborty M. Management of respiratory distress syndrome in preterm infants in wales: a full audit cycle of a quality improvement project. Scientific reports. 2020 Feb 26;10(1):1-7.
- Soleimani F, Zaheri F, Abdi F. Long-term neurodevelopmental outcomes after preterm birth. Iranian Red Crescent Medical Journal. 2014 Jun;16(6).
IMPORTANT NOTICE: MOTHER’S MILK IS BEST FOR YOUR BABY
The World Health Organization (WHO)* has recommended that pregnant women and new mothers be informed of the benefits and superiority of breast-feeding, in particular, the fact that it provides the best nutrition and protection from illness for babies. Mothers should be given guidance on the preparation for and maintenance of lactation, with special emphasis on the importance of the well-balanced diet both during pregnancy and after delivery. Unnecessary introduction of partial bottle feeding or other foods and drinks should be discouraged since it will have a negative effect on breast-feeding. Similarly, mothers should be warned of the difficulty of reversing a decision not to breastfeed. Before advising a mother to use an infant formula, she should be advised of the social and financial implications of her decision. For example, if a baby is exclusively bottle-fed, more than one can (500g) per week will be needed, so the family circumstances and cost should be kept in mind. Mother should be reminded that breast milk is not only the best but also the most economical food for babies. If a decision to use infant formula is taken, it is important to give instruction on correct preparation methods, emphasizing that unboiled water, unsterilized bottles or incorrect dilution can lead to illness.
*See: International Code of Marketing of Breast Milk Substitutes, adopted by the World Health Assembly in Resolution WHA 34.22, May 1981.
Importance of Breastfeeding:
Immediately after delivery, breast milk is yellowish and sticky. This milk is called colostrum, which is secreted during the first week of delivery. Colostrum is more nutritious than mature milk because it contains more protein, more anti-infective properties which are of great importance for the infant's defense against dangerous neonatal infections. It also contains higher levels of, Vitamin 'A', (ii) breast miIk- A) is, a complete and balanced food and provides all the nutrients needed by the infant [for the first six months of life] (B) has anti-infective properties that protect the infants from infection in the early months (C) is always available; (D) needs no utensils or water (which might, carry germs) or fuel for its preparation, (iii) breastfeeding is much cheaper than feeding infant milk substitutes as the cost of the extra food needed by the mother is negligible compared to the cost of feeding infant milk substitutes, (iv) mothers who breast-feed usually have longer periods of infertility after child birth than non-lactators; (b) details of management of breast feeding, as under:- (i) breast-feeding- (A) immediately after delivery enables the contraction of the womb and helps the mother to regain her figure quickly; (B) is successful when the infant suckles frequently and the mother wanting to breast-feed is confident in her ability to do so (ii) in order to promote and support breast-feeding the mother’s natural desire to breast feed should always be encouraged by giving, where needed, practical advice and making sure that she has the support of her relatives. (iii) adequate care for the breast and nipples should be taken during pregnancy. (iv) it is also necessary to put the infant to the breast as soon as possible after delivery, (v) let the mother and the infant stay together after the delivery, the mother and her infant should be allowed to stay together (in hospital, this is called "rooming-in"); (vi) give the infant colostrum as it is rich in many nutrients and anti-infective factors protecting the infants from infections during the few days of its birth; (vii) the practice of discarding colostrum and giving sugar water, honey water, butter or other concoctions instead of colostrum should be very strongly discouraged; (viii) let the infants suckle on demand; (ix) every effort should be made to breast-feed the infants whenever they cry; (x) mother should keep her body and clothes and that of the infant always neat and clean. Breast-feeding is the best form of nutrition for babies and provides many benefits to babies and mothers. It is important that, in preparation for and during breast-feeding, you eat a healthy, balanced diet. Combined breast and bottle-feeding in the first weeks of life may reduce the supply of your own breast-milk and reversing the decision not to breast-feed is difficult. Always consult your Healthcare Professional for advice about feeding your baby. The social and financial implications of using infant formula should be considered. Improper use of an infant formula or inappropriate foods or feeding methods may present a health hazard. If you use infant formula, you should follow manufacturer's instructions for use carefully - failure to follow the instructions may make your baby ill.
IMPORTANT NOTICE
Breast milk is best for babies. At Danone, we support breast feeding and believe that breast milk is the best food for babies as the sole source of nutrition for the first 6 months of life and is recommended to be continued until 2 years with the introduction of appropriate complementary foods after 6 months of age.
IMPORTANT NOTICE: Breastfeeding is the best for babies and a healthy diet / maternal nutrition is important when breastfeeding. A decision not to breastfeed can be difficult to reverse. Infant formula is suitable from birth when babies are not breastfed. It is recommended that all formula milks be used on the advice of a doctor, midwife, health visitor, public health nurse, dietitian, pharmacist, or other professional responsible for maternal and child-care and the financial implications should be considered. All preparation and feeding instructions should be followed carefully as inappropriate preparation could lead to health hazards.
CVM code: 1635577590269
How did you find the article? Vote Now
AWESOME
GOOD
OK
NOT SO GOOD
FAIL
Recent Articles
Preterm Infants Born too Soon

Preterm birth (PTB) is defined by the World Health Organization (WHO) as the birth of a baby before...
LCPUFA Supplementation in Pre-term Infants: Is it required?

By- Danone Nutricia Academy
Experts
Docosahexaenoic acid (DHA), a long chain polyunsaturated fatty acid (LCPUFA), is necessary for cogn...





